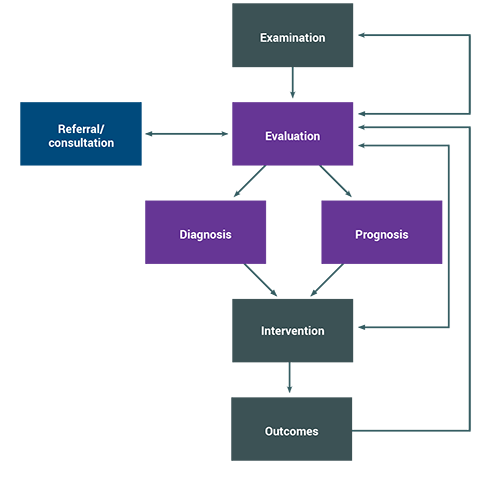
The initial physical therapist visit consists of an examination and evaluation. Typically, these are completed in one visit, but they may occur over two or more visits.
Documentation elements for the initial examination and evaluation include the following: history (including review of systems), physical examination, tests and measures, diagnosis, prognosis, management plan, and plan of care.