The advent of 3-dimensional (3D) printers in the 1990s led people to dream about what someday could be accomplished, especially in health care. Physical therapists (PTs) were among those with big ideas about what might be possible for their profession. In less than 30 years, many of those concepts are coming to fruition.
Today, 3D printing is being used to customize assistive devices, modify special equipment, and create specific adaptations for equipment or exercises. In audiology, for example, hearing aids are manufactured almost exclusively using 3D printing.1 And many PTs are finding that using a 3D printer can move a clinic ahead in a competitive environment.
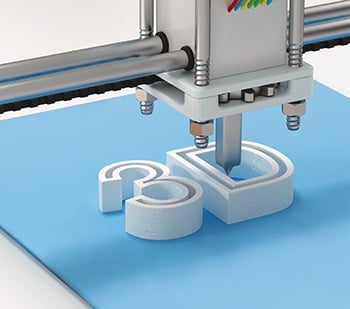
At its most basic, 3D printing begins with a digital model—a type of computer program. The printer then turns that digital model into a physical object—often but not always mechanical parts—by adding materials layer by layer. (See "What is 3D Printing?" on page 29.)