Administrative requirements imposed by payers continue to significantly burden physical therapists and negatively impact patient care, according to APTA's third and most recent survey on administrative burden.
Among the key findings:
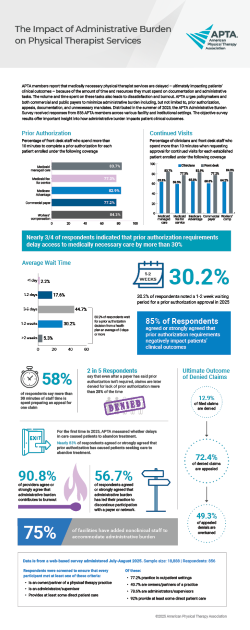
- Wait times for prior authorization have escalated steadily over the last seven years, with 30% of survey respondents waiting one to two weeks for prior authorization approval.
- Prior authorization requirements negatively impacted patients' clinical outcomes, according to 85% of respondents. A similar number, 83%, of respondents agreed or strongly agreed that prior authorization has caused their patients to abandon treatment.
- In the latest survey, 75% of respondents said they had to hire administrative staff to keep up with the administrative demands.
- A majority of respondents, 57%, agreed or strongly agreed that administrative burden has led their practice to discontinue participation with a payer or network.
You can join APTA in fighting to reduce administrative burdens by using the infographic and report to:
- Show payers that excessive and unnecessary administrative requirements harm outcomes and discourage patients from accessing care.
- Urge lawmakers to require transparency, consistency, and timeliness in payer processes.
- Demonstrate for payers, regulators, and policymakers how administrative burden fuels provider burnout and undermines patient outcomes.
Members can join the APTA Advocacy Network for a closer look at APTA's advocacy efforts and to connect with other members working for change. Contact APTA’s advocacy staff with any questions or to share how you've used the infographic and report for advocacy.